AACR Annual Meeting 2019: Manipulating the Immune System in Cancer Therapy
Cancer immunotherapy research has exploded in recent years. This treatment utilizes a patient’s own immune system to recognize and attack cancer cells. While many successful immunotherapeutic regimens have relied on checkpoint inhibition, other immunotherapeutic approaches, such as adoptive cellular therapies (ACT), the use of bispecific antibodies, and targeting components of the tumor microenvironment, are showing promise in a variety of cancer types.
The third plenary session of the AACR Annual Meeting 2019, titled “Manipulating the Immune System in Cancer Therapy,“ focused on recent advances in the field of immunotherapy. This session was chaired by Padmanee Sharma, MD, PhD, professor in the Department of Genitourinary Medical Oncology at The University of Texas MD Anderson Cancer Center, who opened the plenary by highlighting the incredible breakthrough of checkpoint inhibitors, which are helping many patients to have durable responses. “We now need to know how we can improve the current immunotherapy strategies so that not only a subset of patients respond, but even more patients can benefit from these therapies,” Sharma said.
Harnessing the power of adoptive cellular therapy
To kick off the session, Sharma introduced Steven Rosenberg, MD, PhD, chief of surgery at the National Cancer Institute, to deliver his talk, “T-cells targeting unique cancer mutations.”
Several types of ACT round out the immunotherapy arsenal, including chimeric antigen receptor (CAR) T-cell therapy, T-cell receptor (TCR) therapy, and tumor-infiltrating lymphocyte (TIL) therapy. These strategies rely on the isolation of T cells, which are either genetically modified to target tumor-specific antigens or are expanded from an endogenous population that recognizes tumor neoantigens. These techniques were explained in detail in a previous post on this blog.
Unlike CAR T-cell therapy or TCR therapy, which modifies T cells taken from the blood, TIL therapy utilizes T cells that have infiltrated the tumor stroma, which requires a tumor biopsy. Tumor-specific T cells are identified, expanded, and infused into the lymphodepleted patient, where they can help mediate tumor regression.
Rosenberg spoke of the benefit of TIL therapy in patients with metastatic melanoma. In 194 consecutive patients treated with this therapy, the overall response rate was 55 percent, with 24 percent of patients achieving a complete response. Of these complete responders, over 95 percent have had ongoing responses from 14 to 152 months.
To improve this therapeutic strategy, Rosenberg and colleagues developed a method to identify the exact antigens that the T cells could recognize. Briefly, tumor-specific neoantigens, identified by sequencing DNA from the tumor biopsy, are inserted into autologous antigen-presenting cells (APCs); neoantigens that elicit T-cell responses are identified as immunogenic. This method allows for improved identification of immunogenic neoantigens beyond those identified by prediction algorithms, and could potentially be applied to all cancer patients – with the caveat that it would be highly individualized and therefore complex, Rosenberg noted. This approach has proven efficacious in some patients with epithelial cancers, and has been shown to synergize with checkpoint inhibition.
While most of the neoantigens identified through these screening efforts have been unique, a few were common neoantigens that correspond to “hotspot mutations” in KRAS and p53, two genes that are frequently mutated in cancer. Rosenberg is beginning to develop a library of TCRs that can recognize shared mutations in the hope of utilizing them for TCR T-cell therapy for patients across a variety of tumor types, especially those with common epithelial cancers.
Bispecific antibodies for T-cell redirection
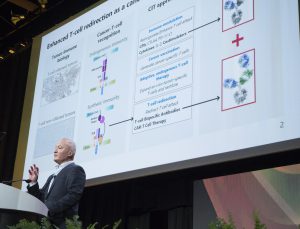
Sharma next introduced Pablo Umana, PhD, head of Research at the Roche Innovation Center in Zurich, to speak about “Redirecting T cells for cancer immunotherapy using next-generation bispecific antibodies and targeted costimulation.”
T-cell bispecific antibodies (TCBs), as the name suggests, are antibodies that are engineered to recognize two distinct antigens: One antigen is present on a T cell (typically CD3, an essential component of the TCR), while the other antigen is present on a tumor cell. In principle, a bispecific antibody is designed to bring a T cell and a tumor cell into close proximity to one another, enabling the T cell to engage and destroy the tumor cell. Additionally, TCBs enhance T cell proliferation and recruitment, Umana noted.
Umana explained that the history of TCBs spans back to 1985, when the bispecific drug catumaxomab was described as recognizing CD3 and epithelial cell adhesion molecule (EpCAM), whose expression is often elevated in epithelial cancers. However, because catumaxomab has an active Fc portion, this can result in off-target reactions, Umana explained. The sole bispecific antibody approved by the U.S. Food and Drug Administration (FDA) for cancer treatment is blinatumomab (Blincyto), which can be used as a treatment for some patients with B-cell acute lymphoblastic leukemia (ALL); its antigen targets are CD3 and CD19, and it does not have an Fc portion, which limits its half-life, Umana noted.
Current TCB strategies, Umana explained, utilize a “silent” Fc antibody portion, which extends the half-life of the drug without off-target side effects. Umana and colleagues are engineering their TCBs so that two portions of the antibody recognize the tumor-specific antigen, while one portion of the antibody recognizes the T cell. This “2:1” format increases the binding to tumor cells, thereby increasing the drug’s therapeutic capacity, said Umana.
Umana presented preclinical data and phase I clinical trial results for two TCBs engineered with the 2:1 format. A 2:1 CD20-CD3 TCB with or without obinutuzumab pretreatment was tested in patients with relapsed/refractory B-cell non-Hodgkin lymphoma. Results from this trial indicate that the toxicities of the treatment are manageable, and some patients saw durable complete responses. A 2:1 CEA-CD3 TCB in combination with the PD-L1 inhibitor atezolizumab was tested in patients with previously treated metastatic colorectal adenocarcinoma. Results from this trial showed encouraging anti-tumor efficacy, both with the TCB alone and in combination with checkpoint inhibition.
Umana wrapped up his presentation by illustrating the use of a TCB which binds to 4-1BBL and fibroblast activation protein (FAP), either alone or in combination with the CEA-CD3 TCB. Umana explained that 4-1BB agonism helps to modulate the tumor microenvironment, reinvigorating T-cell responses. The combination of multiple TCBs shows preclinical efficacy and warrants further investigation in this field, Umana concluded.
Strategies to target immunosuppressive macrophages
Sharma introduced Judith Varner, PhD, professor in the departments of Pathology and Medicine at University of California San Diego School of Medicine, to talk about “Taming the beast: Strategies to target the immune-suppressive macrophage to enhance cancer immune therapy.”
Varner explained that the immunosuppressive macrophage, “the beast of the tumor microenvironment,” is a major driver of T-cell exclusion from tumors, resulting in immunologically ignorant tumors that are not likely to respond to checkpoint inhibitors. Immunosuppressive macrophages have been shown to outnumber tumor cells, and macrophage enrichment is associated with a poor prognosis.
There are two types of macrophages – M1 macrophages respond to pathogens or injury, stimulate the immune system, and enhance T-cell recruitment, while M2 macrophages are involved in wound healing, immune suppression, and angiogenesis. Most macrophages in the tumor microenvironment are of the M2 phenotype, Varner noted.
An important goal in the field is to identify ways to inhibit macrophage-mediated immune suppression. Potential methods to inhibit this process include impeding macrophage accumulation in the tumors, and repolarizing macrophages in the tumor microenvironment from the M2 to the M1 phenotype. To this end, Varner and colleagues previously found that the PI3-kinase isoform PI3Kγ promotes myeloid cell recruitment to tumors, and that genetic or pharmaceutical inhibition of PI3Kγ blocked tumor growth in mouse models of multiple cancer types. Additionally, they found that the inhibition of PI3Kγ facilitates immunostimulatory cytokine expression and restores T-cell cytotoxicity.
Because the inhibition of PI3Kγ was shown to synergize with anti-PD-1 immunotherapy in preclinical models, a phase I clinical trial is evaluating the PI3Kγ inhibitor IPI-549 as a monotherapy or in combination with the anti-PD-1 immunotherapeutic nivolumab in patients with advanced solid tumors. Initial results demonstrated early efficacy for some patients, with biomarker analyses indicating a reduction in circulating myeloid-derived suppressor cells (MDSCs) and an increase in exhausted T-cell proliferation for patients in the monotherapy expansion cohort. Varner noted that IPI-549 will be moving into phase II clinical trials.
To conclude her talk, Varner spoke about the difference between bone marrow-derived macrophages (BMDM) and tissue-resident macrophages (TRM). Unlike BMDM, TRM are highly proliferative and immunosuppressive, explained Varner. CDK and KIT inhibition can suppress TRM proliferation in vitro, and the treatment of murine cancer models with a KIT inhibitor decreases tumor burden, identifying a potential way to selectively target these immunosuppressive macrophages in the setting of cancer.
Biomarkers for response to immune checkpoint inhibition
Sharma introduced the final speaker, Dung Le, MD, associate professor of oncology at Johns Hopkins Sidney Kimmel Comprehensive Cancer Center, who discussed “Mismatch repair deficiency: A connection between the immune system and cancer genetics.”
Le began her talk by emphasizing the need for predictive biomarkers to facilitate the identification of patients who will benefit from treatment with checkpoint inhibitors. While PD-L1 expression is often used for this purpose, other predictive biomarkers, such as tumor mutational load or the expression of inflammatory signatures, are being utilized.
The DNA mismatch repair (MMR) system is responsible for finding and correcting aberrant mutations that arise due to DNA replication or DNA damage. Mutations to genes in the MMR system can result in high microsatellite instability (MSI). Tumors that are MMR-deficient and/or MSI-high can have a high tumor mutational burden (TMB); these hypermutated tumors can elicit an immune response, often rendering them susceptible to checkpoint inhibition. While several tumor types have been shown to have MMR deficiency, colorectal tumors are the most likely to harbor this feature.
Le spotlighted some of the clinical trials that led to the landmark tissue-agnostic approval of the anti-PD-1 therapeutic pembrolizumab for the treatment of patients with MSI-high or MMR-deficient cancers. A summary of these trials and a detailed explanation of this approval was covered previously on this blog.
Next, Le highlighted recent results from a subgroup of patients in the Checkmate-142 trial; MSI-high colorectal patients were treated with a combination of the anti-PD-1 therapeutic nivolumab (Opdivo) and the anti-CTLA-4 therapeutic ipilimumab (Yervoy) as first-line treatment. The overall response rate for these patients was 60 percent, with 7 percent achieving a complete response and 53 percent achieving a partial response. Le also spoke about results from a subgroup of patients in the NICHE trial; colorectal cancer patients were preoperatively treated with the same drug combination. All patients with MMR-deficient colorectal cancer had a major pathological response, while no major pathological responses were observed in patients with MMR-proficient colorectal cancer.
At the end of her talk, Le spoke about using next-generation sequencing (NGS) methods to determine MSI status from cell-free DNA (cfDNA), which could allow for serial sampling and could be used when tissue samples are limited or not available.
Improving patient survival by supplementing checkpoint blockade
To close the session, Sharma briefly spoke to these immunotherapeutic strategies, and how they all synergized with checkpoint inhibition. “All of these next steps, I think, will certainly benefit our patients as we see improved overall response rate and improved survival of our patients as a result of rational combination strategies based on the great science that you heard today,” she noted.