How Can We Turn “Cold” Pancreatic Tumors “Hot”?
Pancreatic cancer remains a challenging disease to treat, with a five-year survival rate of less than 9 percent, according to recent statistics. Unlike many other cancers, which can now be treated with checkpoint blockade immunotherapy, pancreatic cancer often does not respond to this type of treatment. One potential reason for this lack of efficacy is that pancreatic tumors tend to be nonimmunogenic, meaning that the cancer fails to elicit a strong immune response.
This issue was the focus of the keynote lecture that opened up the AACR Tumor Immunology and Immunotherapy meeting, which took place last week in Miami. Elizabeth M. Jaffee, MD, FAACR, deputy director of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins and President of the AACR, spoke about how we can use cancer vaccines to supplement the treatment of pancreatic cancer.
“[Pancreatic cancer] is not one of the cancers that naturally respond[s] to immunotherapy, but I’m going to hopefully convince you that it is possible to turn this cancer that’s really not immunogenic into one that is susceptible to immunotherapy,” said Jaffee.
How do cancer vaccines work?
Unlike traditional vaccines, which are used to prevent a specific disease, cancer treatment vaccines are used to stimulate the immune system to target and attack a pre-existing cancer. Cancer treatment vaccines are often built with two components—tumor-specific antigens, so that the T cells can identify what molecules they should target, and an immunostimulatory adjuvant, which helps to enhance the immune response.
Currently sipuleucel-T (Provenge), a therapeutic for patients with advanced hormone-refractory prostate cancer, is the sole vaccine approved by the U.S. Food and Drug Administration (FDA) for the treatment of cancer. GVAX is a type of cancer vaccine that is being investigated in multiple clinical trials, many of which are evaluating its use in the treatment of pancreatic cancer. GVAX is a whole-cell tumor vaccine that utilizes irradiated cancer cells that have been genetically modified to secrete the cytokine GM-CSF. Another type of cancer vaccine utilizes neoepitopes identified in individual cancers; a pair of studies, published in Nature, have investigated this approach in patients with melanoma.
Cancer vaccines for non-immunogenic tumors
“We’ve been testing the hypothesis that a naturally nonimmunogenic cancer, like pancreatic cancer, requires at least two steps in order to induce an optimal immune response,” said Jaffee. “The first step is to activate a good T cell.”
Jaffee is investigating the use of vaccines to activate T cells. Other researchers have stimulated T cells with chemotherapy or radiation, which can release antigens through cancer-cell death and also enhance antigen presentation. “There are multiple different approaches, but the goal here is to first induce a good T cell,” Jaffee explained.
Jaffee discussed reprogramming immune responses following T-cell activation by stimulating T-cell agonists and inhibiting immunosuppressive signals. Activating receptors, such as OX40, can be stimulated with agonistic antibodies, while inhibitory receptors, such as CTLA-4 and PD-1, can be suppressed with blocking antibodies. Both of these pathways may need to be modulated in some difficult-to-treat cancers, Jaffee noted.
One recent area of research for Jaffee is the investigation of neoantigen vaccines as a first step to activate T cells.
Utilization of neoepitope vaccines in a pancreatic mouse model
Pancreatic cancer does not have a high mutational burden, noted Jaffee. Rather, this tumor type has an intermediate mutational burden, with about “30 to 60 expressed mutations per cancer,” she said. “So we wanted to ask—can we use a neoepitope-targeted vaccine?”
In this type of vaccine, tumors are sequenced, mutations are identified, and a vaccine is generated that targets neoantigens specific to that cancer, explained Jaffee. In a recent study, Jaffee evaluated the preclinical viability of 12 neoantigen-targeted peptide vaccines in a pancreatic mouse model. Peptide neoantigens had the largest T-cell response when coupled with stimulator of interferon genes (STING) as an adjuvant.
Jaffee and colleagues also investigated the incorporation of the neoantigen vaccine in a combinatorial treatment with an OX40 agonist and a PD-1 inhibitor. They found that the inclusion of all three of these elements in the treatment of the mice resulted in the best outcomes, as measured by reduction in tumor size and reduction in the expression of T-cell exhaustion markers. Furthermore, mice treated with all three agents were more likely to remain tumor-free if rechallenged with pancreatic tumors compared to mice treated with the vaccine and the OX40 agonist or the vaccine and a PD-1 inhibitor. This suggests that “memory responses may need some other signals in addition to anti-PD-1,” noted Jaffee.
The results of this study will initiate a pilot trial investigating the combinatorial efficacy of all three therapeutics in patients with advanced pancreatic and microsatellite stable colorectal cancers, noted Jaffee.
Emerging technologies to guide combinatorial immunotherapy treatments
In a prior study, Jaffee and colleagues evaluated the use of GVAX either alone or in combination with low-dose cyclophosphamide, a common chemotherapy drug that suppresses the immune system, in patients with resectable pancreatic ductal adenocarcinoma (PDAC). Patients received up to six intradermal treatments of GVAX, with the first injection administered two weeks prior to surgery. Following surgery, patients received adjuvant chemotherapy and chemoradiation and additional treatments with the vaccine.
Analysis of the resected tumors showed that the majority of patients developed intratumoral tertiary lymphoid aggregates in response to treatment with GVAX, suggesting that the vaccine can trigger an adaptive T-cell reaction within the tumor. Jaffee and colleagues also determined that the lymphoid aggregates are sites of immune activation and regulation, which was evidenced by the abundant expression of the early T-cell activation marker, CD69, and the T cell trafficking maker CXCR3, among others.
Importantly, “…in patients who went on to have long-term disease-free survival…we also saw that CD8 T cells came out of those lymphoid aggregates, infiltrated the tumor, and they were very activated,” noted Jaffee.
To further interrogate biomarkers associated with long-term survival, Jaffee collaborated with Lisa Coussens, PhD, from the Oregon Health & Sciences University School of Medicine to utilize multiplex immunohistochemistry to simultaneously evaluate multiple biomarkers in a single sample.
In a recent study, Coussens, Jaffee, and colleagues evaluated lymphoid and myeloid cell densities in PDAC tumors following GVAX treatment. The researchers observed that PDAC samples with a high myeloid-inflamed status were associated with a shorter overall survival. They also found that PD-L1 upregulation in myeloid cells was associated with activated cytotoxic T cells, which was correlated with a better prognosis.
Jaffee and colleagues are also beginning to utilize T-cell receptor (TCR) sequencing to identify features associated with long-term survival in patients with pancreatic cancer. In a recent study, Jaffee and colleagues evaluated TCR repertoires in the peripheral blood from metastatic pancreatic cancer patients treated from studies evaluating CTLA-4 blockade (ipilimumab) with or without GVAX, or GVAX and the immunostimulant CRS-207 with or without PD-1 blockade (nivolumab). They found that TCR repertoires were differentially affected by these two treatments, and illustrate that TCR sequencing may aid in the identification of pancreatic cancer patients with clinical response to immunotherapeutic treatment.
These results have led to an ongoing clinical trial that is investigating the efficacy of nivolumab, ipilimumab, and CRS-207 with or without GVAX treatment (along with cyclophosphamide) in patients with advanced pancreatic cancer.
Final thoughts
“We really have to be more precision-based in our immunotherapies, even with our checkpoints,” Jaffee said. She envisions having treatment plans for patients that are reflective of the temporal changes in the tumor microenvironment.
“Precision immunotherapy is something that we really need to be doing more in the clinics,” Jaffee concluded.
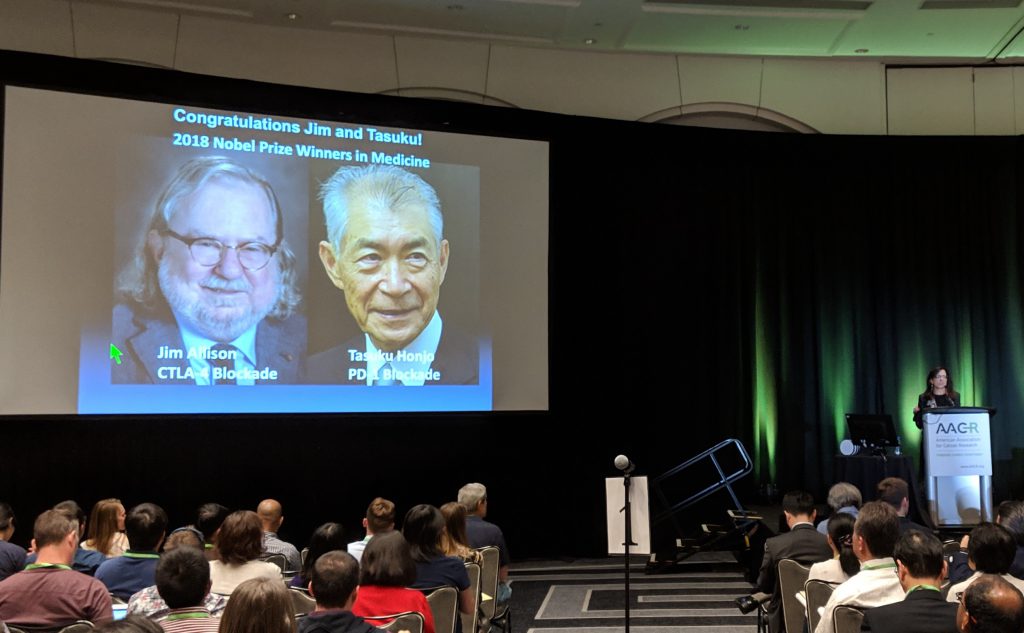
Jaffee congratulated the two recent Nobel laureates in Physiology or Medicine, James Allison, PhD, FAACR, and Tasuku Honjo, MD, PhD, for their achievements in the immunotherapy field at her opening keynote lecture in Miami. Photo courtesy of Ashley James.