FDA Approves New Treatments for Three Cancer Types
In November and the first half of December, the U.S. Food and Drug Administration (FDA) announced three approvals for new treatments for several types of cancer. On December 18, the FDA approved the new molecularly targeted therapeutic enfortumab vedotin-ejfv (Padcev) to treat certain patients who have bladder cancer; on November 21, the agency expanded the use of the molecularly targeted therapeutic acalabrutinib (Calquence) to include treating adults who have chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL); and on November 14, it approved the new molecularly targeted therapeutic zanubrutinib (Brukinsa) to treat certain patients who have mantle cell lymphoma.
A new treatment for bladder cancer
Bladder cancer is the sixth most commonly diagnosed cancer in the United States, according to data from the National Cancer Institute (NCI). More than 90 percent of the 80,470 new cases of bladder cancer expected to have been diagnosed in the United States in 2019 will have been classed as urothelial carcinomas because they arose in cells that comprise the transitional cell urothelium that lines the bladder.

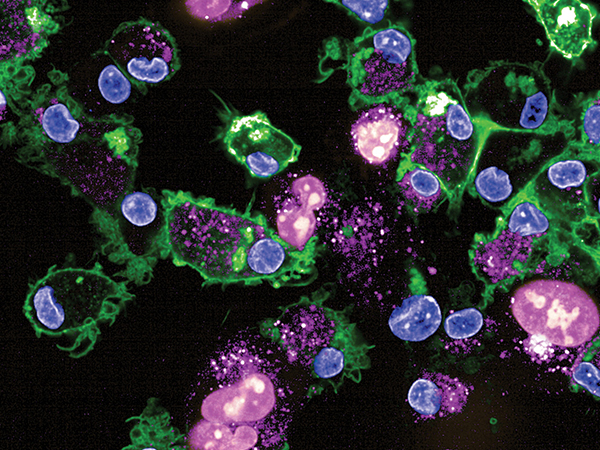
Research, including a paper published in the AACR journal Cancer Research, has shown that up to 60 percent of bladder cancers are characterized by elevated levels of a protein called nectin-4 and that the nectin-4–targeted therapeutic enfortumab vedotin-ejfv causes tumor regression in preclinical models of bladder cancer.
Enfortumab vedotin-ejfv is a type of molecularly targeted therapeutic called an antibody-drug conjugate. It comprises a cytotoxic agent, monomethyl auristatin E, attached to a nectin-4–targeted antibody by a linker. When the antibody attaches to nectin-4 on the surface of bladder cancer cells, the antibody-drug conjugate is internalized by the cells. This leads to monomethyl auristatin E being released from the linker and antibody. Once free, the monomethyl auristatin E is toxic to the bladder cancer cells, which ultimately die.
The approval of enfortumab vedotin-ejfv is for treating adults who have locally advanced or metastatic urothelial cancer that has progressed despite treatment with an immune checkpoint inhibitor and a platinum-containing chemotherapy regimen. The approval was based on results from the phase II EV-201 clinical trial that were published recently in the Journal of Clinical Oncology. The results showed that 44 percent of patients had complete or partial tumor shrinkage after treatment with enfortumab vedotin-ejfv.
Targeting non-Hodgkin lymphoma
Non-Hodgkin lymphoma is the most common blood cancer diagnosed in the United States. By the end of 2019, 74,200 people in the United States are expected to have been newly diagnosed with the disease and 19,970 to have died from it, according to data from the NCI.
Most types of non-Hodgkin lymphoma arise in immune cells called B cells. B cells have on their surface a protein complex called the B-cell receptor. In non-Hodgkin lymphoma B cells, the B-cell receptor is constitutively activated, meaning it is constantly triggering multiple downstream signaling pathways that promote the survival and replication of the cancer cells.
Bruton tyrosine kinase (BTK) is a component of the signaling pathways activated by the B-cell receptor, making it a rational therapeutic target for non-Hodgkin lymphomas that arise in B cells, including mantle cell lymphoma, as well as CLL and SLL.
The two molecularly targeted therapeutics recently approved by the FDA, acalabrutinib and zanubrutinib, both target BTK.
Zanubrutinib was approved for treating adults who have mantle cell lymphoma that has progressed despite at least one prior treatment. According to the FDA statement, the approval was based on combined results from a phase II clinical trial involving 86 patients and a phase I/II clinical trial involving 32 patients. In both trials, 84 percent of the patients had partial or complete tumor shrinkage following treatment with zanubrutinib. Complete tumor shrinkage was seen for 59 percent of patients in the larger clinical trial and for 22 percent of those in the smaller clinical trial.
Mantle cell lymphoma is an aggressive form of non-Hodgkin lymphoma. Acalabrutinib was approved by the FDA for treating certain patients with the disease in October 2017, as discussed in a previous post on this blog. The new approval for acalabrutinib is for treating adults with CLL or SLL, which are slow-growing types of non-Hodgkin lymphoma. CLL and SLL are essentially the same disease, according to the NCI, but have different names depending on where in the body the cancer cells accumulate. CLL cells are found mostly in the blood and bone marrow, whereas SLL cells are found mostly in the lymph nodes.
The CLL and SLL acalabrutinib approval was based on results from two randomized phase III clinical trials, the ELEVATE-TN clinical trial, which involved 535 patients with previously untreated CLL or SLL, and the ASCEND clinical trial, which involved 310 patients with CLL or SLL that had relapsed after or not responded to at least one prior treatment. In both clinical trials, the time before disease progressed was significantly longer among patients who received acalabrutinib compared with patients who received alternative treatments.
The approval of acalabrutinib for CLL and SLL was the second approval that the FDA has granted using the agency’s new Project Orbis international collaboration initiative. The first was the September 2019 approval of the immunotherapeutic pembrolizumab (Keytruda) for treating certain patients with endometrial cancer. The international partners that the FDA collaborated with for the acalabrutinib review were the Australian and Canadian regulatory agencies, thereby providing CLL and SLL patients in these countries with earlier access to acalabrutinib.