FDA Approves New Treatments for Colorectal Cancer, Leukemia, and Melanoma
During the early part of summer 2018, the U.S. Food and Drug Administration (FDA) has approved several new anticancer therapeutics and expanded the use of some previously approved anticancer therapeutics to include new types of cancer. Specifically, the agency approved a new combination of molecularly targeted therapeutics—encorafenib (Braftovi) and binimetinib (Mektovi)—for treating certain patients with melanoma. The FDA also approved a new molecularly targeted therapeutic—ivosidenib (Tibsovo)—for treating certain patients with acute myeloid leukemia (AML). In addition, it expanded the use of a combination of immunotherapeutics—ipilimumab (Yervoy) and nivolumab (Opdivo)—to include the treatment of certain patients with colorectal cancer.
These approvals are the culmination of many years of hard work by researchers working in a wide range of disciplines and are a testament to the unceasing progress we are making against cancer.
A new targeted therapy combo for melanoma
Melanoma is not the most common type of skin cancer, but it is the deadliest; almost 10,000 people in the United States are expected to die from the disease in 2018, according to data from the National Cancer Institute (NCI) Surveillance, Epidemiology, and End Results (SEER) program.
The year 2011 ushered in a new era in the treatment of metastatic melanoma. It was the year that that FDA approved the first molecularly targeted therapeutic, vemurafenib (Zelboraf), and the first immunotherapeutic, ipilimumab (Yervoy), for treating this disease. Since then, the FDA has approved several other molecularly targeted therapeutics and immunotherapeutics, all of which have helped improve patient outcomes. For example, the percentage of patients living five or more years after a diagnosis with metastatic melanoma has risen to 22.5 percent from only 15 percent in 2010.
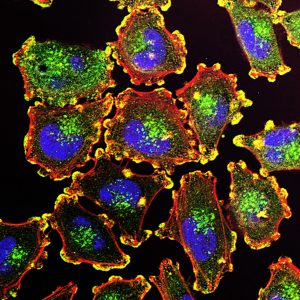
The growth of up to 50 percent of melanomas is driven by mutations in the BRAF gene that are known as BRAF V600 mutations. All the molecularly targeted therapeutics approved for treating metastatic melanoma target either the altered BRAF proteins encoded by BRAF V600 mutations or two proteins that function further downstream in the BRAF signaling pathway, MEK1 and MEK2.
Most patients with metastatic melanoma that tests positive for a BRAF V600 mutation are treated with an FDA-approved combination of molecularly targeted therapeutics, one that targets the altered BRAF proteins generated by BRAF V600 mutations and one that targets MEK1 and MEK2. This is because treatment with the approved combinations—vemurafenib and cobimetinib (Cotellic), and dabrafenib (Tafinlar) and trametinib (Mekinist)—improves patient outcomes compared with treatment with the BRAF-targeted therapeutics alone.
The FDA approved a third combination of molecularly targeted therapeutics, encorafenib (Braftovi) and binimetinib (Mektovi), on June 27, 2018. Encorafenib targets BRAF proteins generated by BRAF V600 mutations and binimetinib targets MEK1 and MEK2. The combination was approved specifically for treating patients with unresectable or metastatic melanoma that tests positive for a BRAF V600E or V600K mutation with an FDA-approved test.
The approval was based on results from the COLUMBUS phase III clinical trial that were published recently in Lancet Oncology. The results showed that the median progression-free survival for patients treated with the combination of encorafenib and binimetinib was more than double that for those treated with vemurafenib. Median progression-free survival was 14.9 months among those receiving encorafenib and binimetinib versus 7.3 months among those receiving vemurafenib.
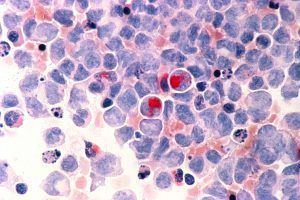
A new molecularly targeted therapeutic for AML
With 10,670 deaths from AML expected to occur in the United States in 2018, according to data from the NCI SEER program, it causes more deaths than any other type of leukemia.
It is only recently that the promise of precision medicine became a reality for patients with AML. As discussed in a previous post on this blog, the FDA approved the first molecularly targeted therapeutic for AML, midostaurin (Rydapt), at the end of April 2017. The second, enasidenib (Idhifa) was approved just a few months later.
The development of these molecularly targeted therapeutics stemmed from research into the biology of AML, in particular the genetic mutations that promote its development. Midostaurin and enasidenib target the proteins encoded by two of the most commonly mutated genes in AML, FLT3 and IDH2, respectively.
IDH1 is another gene mutated in a significant proportion of AML cases, making the altered proteins produced by mutations in this gene a rational therapeutic target. These are the proteins targeted by ivosidenib.
Ivosidenib was approved by the FDA on July 20, 2018, for treating adults with AML that has not responded to or has relapsed after other treatments, and that harbors a mutation in the IDH1 gene. The approval was based on results from a phase 1 clinical trial, some of which were published recently in The New England Journal of Medicine. The results showed that more than 30 percent of patients treated with ivosidenib had complete remission, meaning that there was no evidence of disease, with either full or partial recovery of blood counts. These responses lasted for a median of 8.2 months.
An immunotherapy combo for colorectal cancer
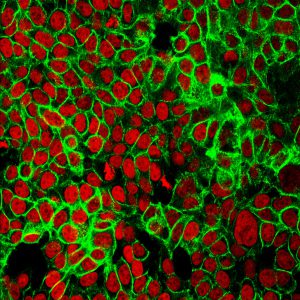
Colorectal cancer is the second most common cause of cancer death in the United States; according to data from the NCI SEER program, 50,630 people are expected to die from the disease in 2018.
Researchers estimate that about 15 percent of the colorectal cancer cases diagnosed in the United States are characterized by a biomarker called microsatellite instability–high because of a DNA mismatch repair deficiency. Cancers that are microsatellite instability–high have been shown to be responsive to treatment with two immunotherapeutics that work by taking the brakes off immune cells called T cells: pembrolizumab (Keytruda) and nivolumab. This led to the FDA approval of pembrolizumab for treating any unresectable or metastatic solid tumor found to be microsatellite instability–high or mismatch repair–deficient, including microsatellite instability–high or mismatch repair–deficient colorectal cancer, in May 2017, and to the FDA approval of nivolumab for treating microsatellite instability–high or mismatch repair–deficient colorectal cancer in August 2017.
On July 10, 2018, the FDA approved nivolumab in combination with ipilimumab for treating patients with metastatic colorectal cancer that is positive for either microsatellite instability–high or mismatch repair deficiency and that has progressed following treatment with a cytotoxic chemotherapy cocktail of fluoropyrimidine, oxaliplatin, and irinotecan.
According to the FDA statement, the approval was based on results from the phase II CheckMate 142 clinical trial that showed that 46 percent of the 82 patients in the trial who were treated with the nivolumab/ipilimumab combination had partial or complete tumor shrinkage. For 89 percent of these patients, the tumor shrinkage lasted six months or longer. These results compare favorably with earlier data from 56 patients who received only nivolumab; 28 percent of these patients had partial or complete tumor shrinkage, with 67 percent of these responses lasting six months or longer.
Anticipating further progress against cancer
There are many other new anticancer therapeutics in the pipeline and we can expect more to be developed as research further deepens our understanding of how cancer arises, develops, and progresses. The staff of Cancer Research Catalyst looks forward to keeping you up to date with the advances as they occur.