FDA Approvals Provide New Advances Against Bladder, Lung, and Kidney Cancer
During late March and early April, the U.S. Food and Drug Administration (FDA) made several decisions that have increased the number of treatment options for certain patients with bladder, lung, and kidney cancer. On March 18, 2019, the agency approved the immunotherapeutic atezolizumab (Tecentriq) for treating certain patients with small-cell lung cancer (SCLC). On April 12, 2019, it approved a new molecularly targeted therapeutic—erdafitinib (Balversa)—for treating certain patients with bladder cancer. Then, on April 19, 2019, it approved the immunotherapeutic pembrolizumab (Keytruda) for treating certain patients with kidney cancer.
Combining an immunotherapeutic with chemotherapy for small-cell lung cancer
SCLC accounts for about 15 percent of lung cancers diagnosed in the United States, according to the National Cancer Institute (NCI). This translates to about 34,000 new cases of the disease each year. Unfortunately, most patients (70 percent) are diagnosed with extensive-stage disease, which means the cancer has spread beyond the lung, or the area between the lungs or the lymph nodes above the collarbone to other parts of the body.
Little progress has been made against extensive-stage SCLC over the past two decades. Outcomes for patients diagnosed with extensive-stage SCLC are poor. Even with treatment, median survival is just six to 12 months, says the NCI.
Standard treatment for extensive-stage SCLC includes combination chemotherapy, most commonly a two-agent combination of a platinum-based chemotherapeutic, either cisplatin or carboplatin, together with etoposide. The new approval adds atezolizumab to combination chemotherapy with carboplatin and etoposide for initial treatment of adults diagnosed with extensive-stage SCLC.
As discussed in a recent post on this blog, atezolizumab works by releasing a brake called PD-1 on natural cancer-fighting immune cells called T cells. It prevents a protein called PD-L1 from engaging the PD-1 brake, thereby freeing T cells to destroy cancer cells. The rationale for adding atezolizumab to standard combination chemotherapy for extensive-stage SCLC was that the disease is characterized by a high mutation rate. Cancers with high mutation rates typically trigger anticancer T cells and can be responsive to immunotherapeutics that release T-cell brakes.
The new approval for atezolizumab was based on results from the randomized, phase III IMPower133 clinical trial. The results, which were published last year in the New England Journal of Medicine, showed that among the 201 patients with previously untreated extensive-stage SCLC who were randomized to atezolizumab, carboplatin, and etoposide, the median overall survival was 12.3 months. The median overall survival was significantly less, 10.3 months, among the 202 patients who were randomized to placebo, carboplatin, and etoposide.
Before this approval for extensive-stage SCLC, atezolizumab was approved for treating certain patients with triple-negative breast cancer in March 2019, for treating certain patients with bladder cancer in May 2016, and for treating certain patients with non–small cell lung cancer in October 2016.
A new molecularly targeted therapeutic for bladder cancer
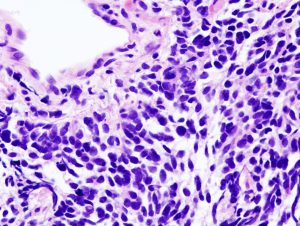
Bladder cancer is the sixth most commonly diagnosed cancer in the United States, according to the NCI. More than 90 percent of the 80,470 new cases of bladder cancer expected to be diagnosed in the United States in 2019 will be classed as urothelial carcinomas because they will arise in cells that comprise the transitional cell urothelium that lines the bladder.
Research, including a paper published in the AACR journal Clinical Cancer Research, has shown that up to 30 percent of urothelial carcinomas have an alteration in one of the four FGFR genes, with the most common alterations being mutations in the FGFR3 gene. These data suggest that targeting FGFRs might provide a new approach to treating urothelial carcinoma.
Erdafitinib is the first FGFR-targeted therapeutic to be approved by the FDA for treating certain patients with urothelial carcinoma. It is intended for patients with locally advanced or metastatic urothelial carcinoma that tests positive for specific FGFR2 or FGFR3 genetic alterations and that has progressed during or after treatment with a platinum-based chemotherapeutic.
The approval of erdafitinib was based on results from the phase II Study BLC2001 clinical trial, according to the FDA. The results showed that 32.2 percent of the 87 patients who received erdafitinib had complete or partial tumor shrinkage. The median duration of these responses was 5.4 months.
The FGFR genetic alterations detected in the tumors of the patients enrolled in the trial were mutations in FGFR3 or gene fusions involving either FGFR2 or FGFR3, according to Janssen Pharmaceutical Companies, which is the company that markets erdafitinib. The FDA approved a new test to detect these and other specific FGFR genetic alterations at the same time as it approved erdafitinib. Use of the new test, which is called the therascreen FGFR RGQ RT-PCR Kit, is required to identify those patients with locally advanced or metastatic urothelial carcinoma for whom erdafitinib is an appropriate treatment option.
Combining an immunotherapeutic and a molecularly targeted therapeutic for kidney cancer
The NCI estimates that there will be 73,820 new cases of kidney cancer diagnosed in the United States in 2019. About 85 percent of these cases will be classified as renal cell carcinoma.
Many patients newly diagnosed with metastatic renal cell carcinoma are first treated with one of several FDA-approved therapeutics that target a number of kinases including VEGF; one of the most commonly used of these therapeutics is sunitinib (Sutent). Another of these therapeutics is axitinib (Inlyta).
The FDA has now approved a new initial treatment for advanced renal cell carcinoma: A combination of axitinib and the immunotherapeutic pembrolizumab, which releases the PD-1 brake on cancer-fighting T cells. The approval was based on results from the randomized, phase III KEYNOTE-426 clinical trial, which were published recently in the New England Journal of Medicine. In short, patients randomized to the combination had significantly improved overall survival rates compared with those randomized to sunitinib. After a median follow-up of 12.8 months, the estimated 12-month survival rate was 89.9 percent for the axitinib plus pembrolizumab combination arm compared with 78.3 percent for the sunitinib arm, which translates into a 47 percent lower risk of death. In addition, the median progression-free survival was significantly longer among those randomized to the combination than it was among those randomized to sunitinib; it was 15.1 months for the combination group versus 11.1 months for the sunitinib group.
Looking to more progress in the future
Clinical trials are the backbone of cancer care, because they provide the evidence for the safety and efficacy of our current treatment armamentarium. With more than 67,000 cancer clinical trials listed on clinicaltrials.gov, it is clear that there is a robust pipeline of new potential approaches to cancer being evaluated in patients. Results from some of these approaches were featured in the more than 200 presentations about exciting clinical trials at the AACR Annual Meeting 2019, held March 29–April 3, and suggest that we can expect to see new anticancer therapeutics developed soon and further expansion in the use of those already in the clinic.