Experts Forecast Cancer Research and Treatment Advances in 2019
In 2018, we witnessed significant momentum in several hot areas of cancer research, including immunotherapy and precision medicine. Researchers have amassed exponential amounts of knowledge in these areas of scientific inquiry in recent years, and 2018 saw many of these gains culminate into innovative treatments for cancer patients.
Overall, in 2018, the U.S. Food and Drug Administration (FDA) approved 18 new cancer therapeutics and expanded the use of 10 previously approved treatments to include new types of cancer. To highlight a few, last year, the FDA approved or expanded the use of five immune checkpoint inhibitors; since 2011, the FDA has approved seven checkpoint inhibitors to treat various solid and hematologic cancers. Last year, the FDA also approved the use of the CAR T-cell therapy tisagenlecleucel (Kymriah) for some patients with non-Hodgkin lymphoma; the second tissue-agnostic cancer therapeutic, larotrectinib (Vitrakvi), to treat patients whose tumors carry specific genetic alterations regardless of organ site; and the PARP inhibitors olaparib (Lynparza) and talazoparib (Talzenna) to treat BRCA gene-mutant breast cancers.
The cancer research community has also been steadfast in its efforts to curb the pandemic of e-cigarettes use among youngsters, with the goal of protecting them from tobacco-related diseases. In response to an alarming increase in the use of e-cigarettes by youth (78 percent and 48 percent increase among high school and middle school students, respectively, between 2017 and 2018), on Nov. 15, 2018, the FDA announced that it will limit most e-cigarette sales to age-restricted, in-person locations, and plans to implement age-verification measures for online sales to restrict minors from buying flavored e-cigarette pods.
Also noteworthy, in May 2018, Congress passed the Childhood Cancer Survivorship, Treatment, Access, and Research (STAR) Act, which was signed into law in June. The Act aims to support pediatric cancer research by expanding the collection of biospecimens and records, improving surveillance, and investigating pediatric survivorship.
What major milestones do experts think we will hit in 2019? We asked Nobel Laureate, Fellow of the AACR Academy, and immunotherapy pioneer James P. Allison, PhD; AACR President-elect and precision medicine expert Elaine Mardis, PhD; and chairperson for the Minorities in Cancer Research Council of the AACR, Brian Rivers, PhD; to share their insights on progress expected in 2019 in the oncology field.
Immunotherapy advances in 2019
“The field of immunotherapy is exploding,” began Allison, professor and chair of the Department of Immunology and executive director of the Immunotherapy Platform at The University of Texas MD Anderson Cancer Center in Houston, Texas. “For the first time, we have several different immunotherapy approaches that are yielding potentially curative treatments for cancer, with some patients remaining cancer-free a decade or more after treatment.”
In 2019, we will start seeing checkpoint blockade combinations come to the forefront, extending the range of cancers that respond to treatment, besides increasing efficacy and response rates, Allison predicts. “I think this is going to be done in a couple of ways,” he notes. One approach is by finding more combinations of immunological agents such as anti-CTLA-4 and anti-PD1/PD-L1 therapies. Other approaches include combinations with chemotherapy, radiation therapy, and genomically targeted drugs. “That is going to greatly improve responses for cancer patients,” he says. By combining checkpoint blockade therapies with agents that are toxic to the cancer cells, it is possible to prime the immune system, but the trick is in carefully choosing the right drugs, given at the right time, to truly optimize effectiveness, he adds. Allison says that it is crucial to study tissue samples from patients to determine why certain combinations work and why some don’t, and these studies should serve as a guide to find the right combinations. “That’s going to be the biggest thing this year,” he notes.
While immune checkpoint inhibitors yield promising results in many patients and in different types of cancer, the responses are limited to roughly a third of cancer patients, and many patients who respond develop resistance to these treatments. “From my viewpoint, there are two types of resistance to immune checkpoint inhibitors,” explains Allison. One is innate resistance in some patients causing failure to respond, which can be overcome, in part, by combining multiple checkpoints or with chemotherapy, radiation, or other approaches. But there are also patients who do not respond because they have acquired defects in gamma-interferon (IFNγ) or beta-2-microglobulin (B2M) signaling, thus losing the ability to respond to the lytic events of IFNγ or the ability to present tumor antigens to immune cells, he says. “I think there are ways around that, involving the development of CD4-targeted agents, particularly using vaccines,” he notes.
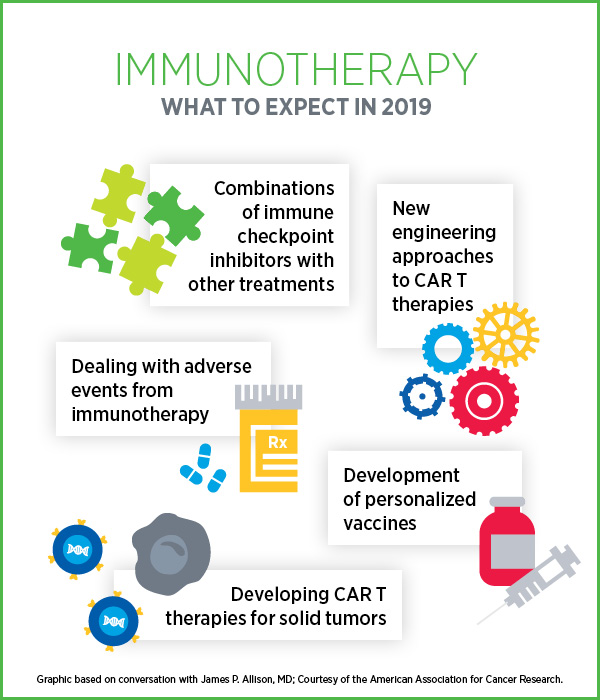
We can expect to see more engineering of CAR T-cell therapies to edit out genes that inhibit T cells, such as PD-1, or to introduce genes that code for the expression of certain cytokines or chemokine receptors, Allison says. “While I expect most efforts to continue to focus on blood cancers for the time being, we will also see approaches using engineered T cells to target solid tumors,” Allison predicts. We will also see more research utilizing proteomics approaches to find antigens and multiple targets co-expressed on tumor cells to guide the use of CAR T-cell therapies, he says.
“In 2019, I hope we will see more studies to address adverse events that are associated with immunological treatment approaches,” Allison says. Understanding adverse events would require extensive analysis of patients’ data and studies of tissue biopsies, and he hopes we will make significant progress in this area.
“The development of personalized cancer vaccines is likely to make a big impact this year,” Allison predicts, with more clinical trials, more studies of genomic sequencing for neoantigen prediction, and studies that address the best way to deliver peptide- and RNA-based vaccines. “I think this area is really going to take off in 2019,” he emphasizes.
“I think the success in recent years with immunotherapy is giving a lot of people, including researchers and patients, some optimism that at least some types of cancer can be cured in some people,” Allison says. “I am very hopeful that we can make immunotherapies work even better. We now know some of the basic rules of the immune system – it’s just a matter of working hard, doing extensive mechanistic studies, and learning from clinical trials that succeed and fail, so we move forward with finding more cures.”
Precision medicine advances in 2019
“We are at a very exciting time right now, especially as we witness the impact of many research studies rolling toward clinical translations,” began Mardis, who is co-executive director of The Institute for Genomic Medicine at Nationwide Children’s Hospital in Columbus, Ohio. “Having been involved with large-scale genomics-based evaluation of tumors in a research setting, it is incredibly gratifying to see the research play out now in the day-to-day reality of cancer patients’ treatments and treatment decisions, all of which lead us to a better understanding of the iconic precision medicine.”
One major ongoing development is the extent of information generated through various genomic clinical assays for patients, Mardis says. While an important outcome of this is the development of therapies that target genomic alterations in the tumors, these initiatives also led to the recognition that certain germline defects can have therapeutic implications. One example is the alterations in the gene BRCA, which invoked the use of PARP inhibitors. Another example is the recognition that MSI-high tumors are indicative of potential response to immune checkpoint inhibitors.
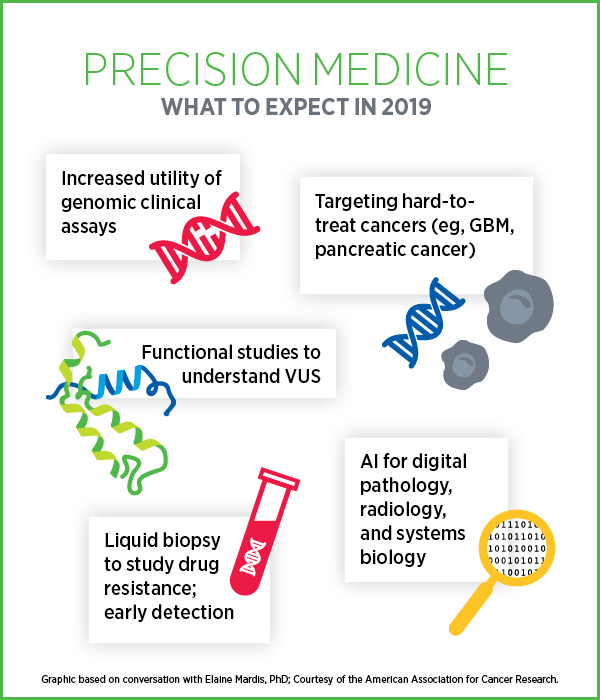
In 2019, we can expect to see more systematic studies that incorporate liquid biopsy-based treatment monitoring to study drug resistance in patients, especially in those with known mutations in their tumors, Mardis notes. Demonstrating the utility of liquid biopsy-based monitoring in detecting treatment resistance can be a stepping stone to use this approach for early detection, she adds.
Mardis is enthusiastic about using artificial intelligence (AI) to aid digital pathology and radiology, but in the coming year, she foresees significant progress in utilizing AI in understanding cancer as a system. “I’m most optimistic about ongoing work across a variety of labs in utilizing AI to study cancer as a system. Some teams are starting to model the information that we generate about cancer systems biology towards the integrative evaluation of tumors,” she notes.
A recent significant development is that many of the hardest targets in cancer, including diseases like glioblastoma multiforme and pancreatic cancer, are starting to get the full focus of innovative research with a clear path to clinical translation, Mardis says. “These tumor types are likely to get a lot of attention in the next few years both in the research space and clinical setting, because they are such hard targets with terrible outcomes for patients.”
“I’m excited about the progress we have made so far in our quest to be more precise in our treatment approaches,” concludes Mardis. “I realize that there are significant hurdles to overcome, especially with difficult-to-treat cancers, but I can’t help but think that with all the intelligence and acquired knowledge that we have today, and the combinatorial approaches to cancer treatment development being tested right now, that we will continue to be successful as we move forward.
“It is a great time to be a part of all of this.”
Cancer prevention and health disparities in 2019
In 2019, we will see an increased focus on implementation science in the areas of prevention and cancer health disparities, says Rivers, who is director of Cancer Health Equity Institute at Morehouse School of Medicine in Atlanta.
Rivers defines implementation science as the systematic study of methods to promote the adoption and integration of evidence-based practices, interventions, and policies related to public health, clinical practice, and community settings. “Implementation science seeks to understand the behavior of health care professionals and other stakeholders as a key variable in the sustainable uptake, adoption, and implementation of evidenced-based interventions and practices,” he explains.
“Tremendous progress has been made in how we address cancer health disparities, but there is still quite a bit of work that needs to be done,” Rivers notes. “The question now is, how do we ensure that there is no gap between the scientific discoveries that we have witnessed in the last decade and the implementation and dissemination of these discoveries to ultimately improve population health?”
He alludes to the gaps that continue to exist in cancer screening among minority and underserved populations. Screening for colorectal cancer has been widely recognized as a strategy that can potentially reduce mortality rates, however, the screening rates in certain underrepresented populations continue to be low for a variety of reasons. “This is where there the tenets of implementation science could help understand the gaps and put forth interventions that were previously adopted and scaled in other groups.”
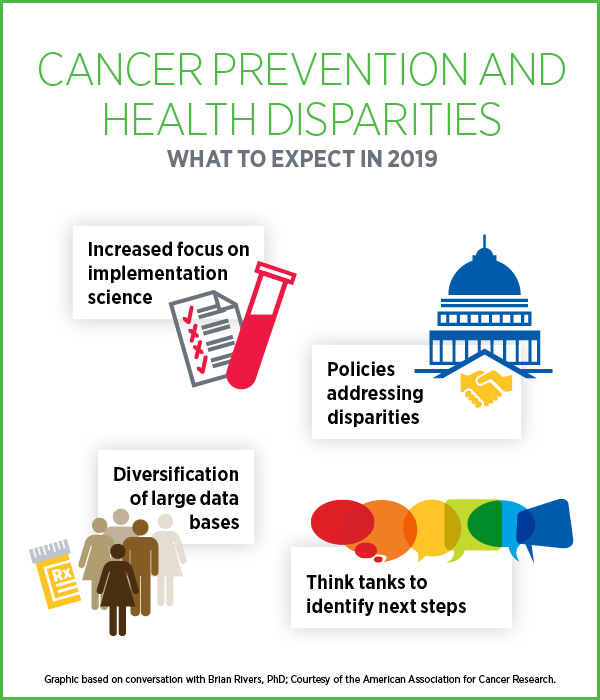
“This year we will see more focus at the policy level as it relates to strategies that address cancer health disparities,” Rivers predicts. “The strength of implementation science is that it takes into account this complex dynamic adaptive system that can be a tremendous resource in guiding cancer health policies, and that’s what is truly needed in the cancer prevention and disparities space to make progress.” The AACR is currently leading the development of the inaugural cancer disparities progress report. This report will help educate the public and Congress on the current state of affairs in cancer health disparities and provide guidance in advancing health equity.
Another area that will get quite a bit of attention in 2019 is the diversification of large databases, Rivers says. Experts in the field are employing strategies for the recruitment and collection of tumor samples from diverse patient populations for cancer genomics studies and ultimately molecular profiling. In March 2018, Morehouse School of Medicine witnessed the launch of an inaugural collaborative initiative known as 2020 by 2020. This initiative is a collaboration of the AACR with several partners, including Pelotonia, through The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute; and M2Gen and the Oncology Research Information Exchange Network (ORIEN).
The goal of 2020 by 2020 is to perform genomic sequencing of tumor and normal tissue of 2,020 African-American cancer patients and aggregate clinical data from these patients by the year 2020 with the purpose of improving our understanding of cancer outcomes in this population.
A strength of the project is the ongoing relationship Morehouse School of Medicine has with medically underserved populations, particularly African-Americans, Rivers says. This collaborative model will be used to establish best practices in engagement that can be extrapolated to other groups and populations in the United States and globally. This initiative will expand the existing African-American cohort already present within the AACR Project GENIE registry, which has made public more than 48,000 genomic profiles to date, with a new release scheduled in early January, Rivers notes. “This initiative is the first one of this type in the country and we are very excited about it.”
Rivers also draws our attention to the Cancer Health Disparities Think Tank that the AACR convened in October 2018, purposed to identify next steps in addressing cancer health disparities. Scientists were invited to speak on three priority areas with the goal of framing future research recommendations for cancer disparities. The priority areas were: increasing the participation of underrepresented populations in clinical trials, development of key resources to accelerate cancer health disparities research to understand the biological basis of disparities, and training the workforce to address cancer health disparities.
“These initiatives are critical to conducting important implementation science research, engaging the community, and ultimately advocating Congress on behalf of cancer research and making progress for cancer patients,” Rivers concluded.





Thank you for this post, but individuals should be aware of symptoms so they can go for testing at initial stages to avoid the severity of the disease.