Complexities of Cancer Explained for Patient Benefit
Editor’s Note: We invite physicians reading this blog to use this post and other resources from the AACR when discussing these issues with patients and their loved ones.
Burgeoning understanding of the biology of cancer has led to advances in cancer prevention, detection, diagnosis, and treatment. These advances mean that a person diagnosed with cancer in the United States today has a greater chance of surviving their diagnosis than ever before.
Despite the tremendous advances, almost 600,000 people in the United States are expected to die from cancer this year alone.
We asked Eric Winer, MD, chief of the Division of Women’s Cancers and director of the Breast Oncology Center at the Susan F. Smith Center for Women’s Cancers at Dana-Farber Cancer Institute in Boston, and professor in the Department of Medicine at Harvard Medical School, to explain for patients and their loved ones how the complexities of cancer make it a hard disease to treat successfully and to talk about efforts to overcome these complexities to reduce the burden of cancer.
What is cancer?
One thing that people sometimes forget is that fundamentally, a cancer is both self and non-self. Cancers arise from cells in our own body, typically because genes are abnormally expressed. When a gene is abnormally expressed, it can lead to the inappropriate production of a protein or to the underproduction of a protein. In turn, this can lead to a series of changes in the cell that transform it into a cancer cell. What distinguishes a cancer cell from a normal cell is that a cancer cell can grow without the normal checks and balances, can invade the surrounding tissues, and can spread to other parts of the body. Importantly, not all cancer cells have the same potential to grow, invade, and spread.
Can you tell us a little more about that fact that cancer is both self and non-self?
Cancers arise within us, often for reasons we don’t understand. Occasionally cancers develop as a result of a virus, such as hepatitis B virus, but more often they develop in response to a toxic substance, such as cigarette smoke, or certain types of chronic inflammation. In many cases, we simply cannot pinpoint a cause. But because cancer develops from what was once a normal cell, this means that cancer cells and normal cells share many common features. For example, cancers need a blood supply to survive but so do all of our normal healthy organs. As you can imagine, this fact has major implications for cancer treatment.
The sharing of characteristics between cancer cells and normal cells is one of the reasons that cancer is sometimes so difficult to treat. It is also one of the reasons why many treatments have so many side effects. We try to take therapeutic advantage of differences between cancer cells and normal cells, but treatment side effects often arise because normal cells are more like cancer cells than we would like. To return to the idea that both cancers and normal organs rely on a blood supply, we have found that drugs that aim to eliminate a cancer by turning off its blood supply can damage normal organs.
What else makes cancer a complex disease?
One of the biggest complexities of cancer is that it is an incredibly diverse disease. There are many different types of cancer, and cancers that arise in different organs often behave very differently. Then, within each organ—for example, the breast or the colon—not all cancers are identical either. In some cases, some cancers that arise in one organ may have more similar characteristics to some cancers that arise in other organs than to other cancers arising in the same organ. For example some cancers arising in the breast might be more similar to some cancers arising in the lung or the ovary than to other breast cancers. This concept is something that we are just beginning to understand.
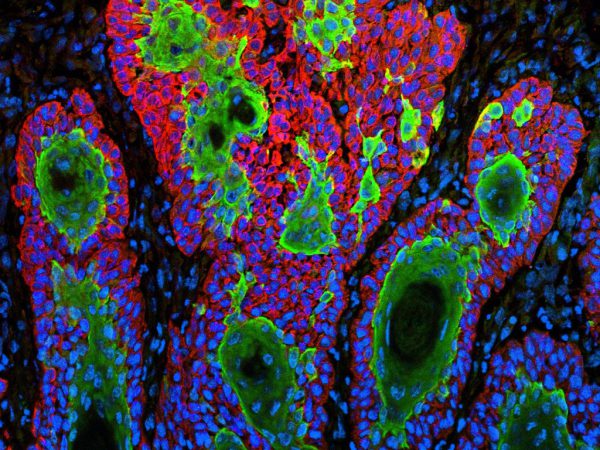
Another complexity is that it is not just about the cancer cells themselves. It also is about how the host, meaning the patient, and the tissue surrounding the cancer cells react to the cancer cells. There is an interplay between the host and the cancer cells, as well as between the environment around the cancer cells (sometimes call the microenvironment) and the cancer cells, that is important in promoting or impeding tumor growth.
How do the complexities of cancer influence precision medicine efforts?
Precision medicine requires that we gain a much finer understanding of an individual’s cancer and the person’s response or reaction to the cancer. To gain this understanding, we may need to sequence the entire genome of a patient’s cancer so that we know which genes are present in altered, or mutated, forms. This knowledge, as well as other molecular information—because we cannot restrict ourselves to genomic analyses alone—can help us understand the real drivers of the behavior of that patient’s cancer. We need to understand what is fueling the cancer’s growth and causing it to spread and threaten the life of the patient so that we can try to intervene with more specific, or more personalized and precise therapies than we have used in the past.
In the end, the process of developing personalized approaches is not simple, largely because cancer is so complex. When we block a pathway, the cancer can often figure out how to use another pathway. Imagine placing a roadblock on a major thoroughfare. At first, the cars back up, but then they find alternate routes. Simply put, many cancers adapt, in much the same way that people adapt. For example, if you tell a person that they cannot drive to work, they figure out a way to overcome this, they walk, they take a bus. In the same way, if you put an obstacle in the path of a cancer, in the shape of a drug, it will often find another route to ensure its survival.
But I don’t want this to sound hopeless, because we have learned a great deal about cancer, which has led to huge successes. The majority of patients who are diagnosed with cancer in the United States are cured of their cancer. Surgery alone or surgery and radiation take care of many, and medical therapy can add to these treatments or sometimes replace these treatments for thousands of others. We have seen real advances in the last few years as we have developed new and better therapies.
Are we able to translate our growing knowledge of the complexities of cancer into clinical advances against cancer?
Right now, we know more about the complexities of cancer than ever before, and we are trying to apply these advances in the clinic. We need to link what we have learned in the lab to what we see in the clinic. We need to use this knowledge to develop new drugs and we need to carefully test these drugs in people. We are looking at a new generation of clinical trials that will increasingly have selection criteria for patient enrollment that include molecular characteristics of patients’ tumors and not just age, disease stage, and number of prior treatments.
One thing that we need to be careful about is: We cannot assume that because a laboratory test detects a specific molecular abnormality in a patient’s tumor that a drug that targets that abnormality will definitely benefit the patient. In fact, our assumptions do not always pan out; for example, drugs that target BRAF prolong survival for patients with BRAF-mutant melanoma but don’t have the same effect for patients with BRAF-mutant colorectal cancer. We cannot go from the cancer laboratory to the pharmacy shelf in one step. Well designed and often complex clinical trials must be done before a drug is ready for primetime use.
We must respect the principles of evidence-based medicine, but we must rethink how we design our clinical trials to make them more nimble and more flexible if we are to better translate our growing knowledge of the complexities of cancer into clinical advances against these diseases. The faster we make these advances, the more patients will be helped, and often cured, in the years ahead.
Eric Winer, MD, has been an AACR member for 10 years.
During this time he has served the AACR in numerous roles, including on the Science Policy and Government Affairs Committee.



Thank you for an easy-to-understand discussion about the complexities of cancer and cancer research.